[blog-divider/]
This e-conversation goes out to about 2,000 people from the industry, our team’s network, and my life. (Thank you LinkedIn.) Over the course of publishing, we have heard from many of you on a broad range of topics.
What we have found fascinating is that different topics generate interest with different people (welcome to the 21st century, Sue); that there is seasonality in your engagement (shocking that the July topics don’t generate as much interaction as do those of other months); and that the topics remain relevant to our strategic work in the industry. (A humble brag, albeit one that I find personally satisfying.)
Last month’s topic concerned my parents’ interaction with the healthcare system and my own roller coaster experience as a result. It generated significant and heartfelt responses from people who had or are currently trying to navigate the system with their own loved ones. I am sorry. You know I feel your frustration and worry.
The comments were particularly poignant because they reminded me that family is everything, everyone has a story, and we experience a merging of our work lives and personal challenges each time someone we love is sick or in need of healthcare.
In addition to sharing some of these comments today – and my responses to them – we also re-share the topics we have covered to date (see the complete list below). We do that not for self-promotion, but rather to acknowledge that this commercialization stuff is hard; we all need reminders and hints regarding core areas where we, as leaders, can make our teams’ lives easier while accomplishing the goal of bringing innovative medicines to patients – the patients whose families are advocating so strongly for them in the comments below.
Finally, in sharing these excerpts with you this month, I am suggesting we keep talking about what we can do to make changes at the system level while also showing each other compassion. We never know what someone is struggling with or worrying about as they show up to work each day. I was humbled to learn what so many of you are going through.
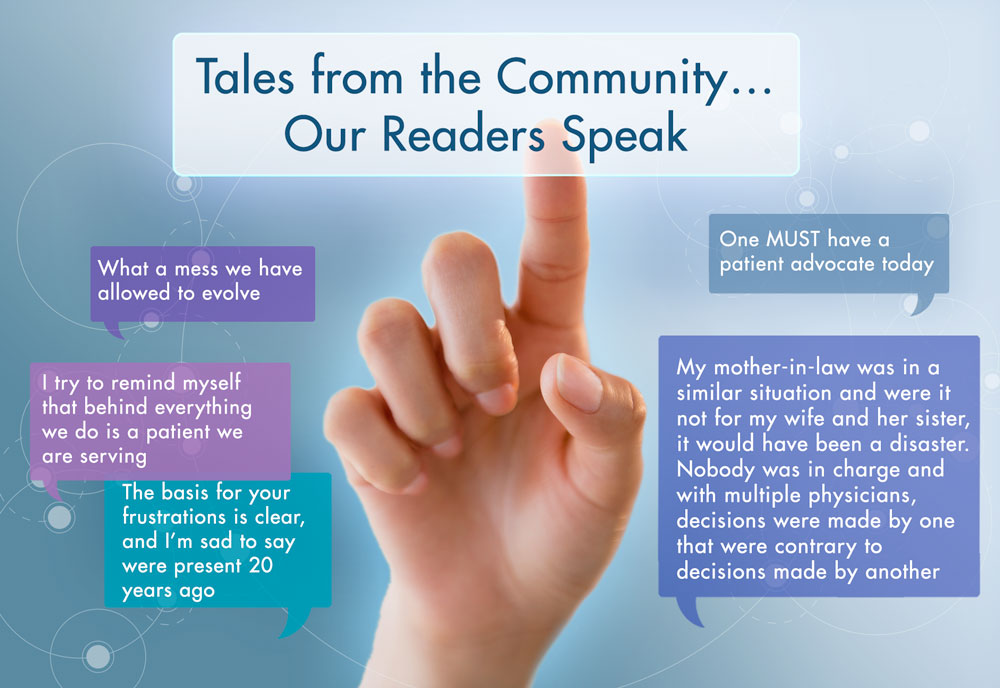
Our Readers Respond
What a mess we have allowed to evolve. I would never choose the word “created” because it’s clear that, like the cow paths of Boston that turned into highways, there was no upfront, integrated planning behind this chaotic mess we call the healthcare delivery “system.” And certainly, no focus on the patient.
Sue’s Thoughts:
I love the cow path analogy! Our current healthcare approach did not anticipate either the volume of “traffic” nor the types of “vehicles” that would one day use that path. One could argue further that while each “driver” is well-intentioned and not the problem, taken together, their unique situation and intentions (goals) only add to the chaos across our outdated infrastructure.
This is where the relevance of the patient and healthcare provider comes in. I do truly believe that the professionals within the system care (I am married to one such individual), and that the patients are willing to tolerate some level of fragmentation. What isn’t sustainable is how it all comes together in a system where patient (and provider) experiences are so frustrating, costs keep increasing, and outcomes are all too variable.
Maybe it is just because I am European, but it feels to me that the Government should play a central role in pushing for your recommendations. The profit motive in healthcare just seems to get in the way – so Government needs to represent the best interests of its citizens to lead the way in terms of a process that delivers coordinated, integrated care.
Sue’s Thoughts:
I found this response so relevant, from both a human and professional perspective. In our work lives, we often talk about shared values and we work to understand each other’s assumptions before drawing a conclusion.
From this person’s response, we infer a belief that healthcare is a right and that government should focus on the best interests (health) of its citizens. Here, both rights and values come into play. Is this a shared assumption in the US?
We also hear a concern about fee-for-service vs. integrated value-based care – an approach that drives volume rather than outcomes. We know that integrated care requires the joint incentives of aligned delivery AND payment models. Hey, that sounds like a policy position on healthcare; access, delivery, and value. I am all for it.
The basis for your frustrations is clear, and I’m sad to say were present 20 years ago when I was still in clinical practice. We talk about evolving and integrating care and navigating through the healthcare system. What are we really doing?? At times I feel these are buzz words that have no basis and foundation.
Sue’s Thoughts:
I wonder if there was a time when the optimism of what “could be” was more upbeat. I felt it when the ACA was making its way through its early challenges. I believed new payment models, patient satisfaction, and new delivery models, like the patient-centered home, had potential.
Was the ACA looking for an audience that wasn’t there or were those concepts not quite ready for the political climate that was to come? I know smart people are trying to figure this out.
We develop a value proposition, tailor it to the various perspectives (hospital, payer, clinician, etc…), support it with data, determine institutional targets, identify key individuals, communicate the story and sit back and count widgets (sales) to determine success. I try to remind myself that behind everything we do is a patient we are serving. But how does that value get translated to the patients [themselves]?
Sue’s Thoughts:
What I love about this response is that it lays out something we could do in biopharma. What if in addition to all of the attention paid to revenues, we also paid attention to the quantifiable impact our products have on patients, providers, and the healthcare delivery systems in which they are used?
Would that additional focus run counter to our primary goal of serving shareholders who want ROI and value creation? How do we make what we do NOT ONLY about the business but also about its impact?
One MUST have a patient advocate today.I do believe our healthcare system is broken and physicians more often than not have their noses in a computer and no longer are clinicians, let alone good diagnosticians.
Sue’s Thoughts:
I include this one because although the observation is true about the demand of electronic medical records and the computers that capture clinicians’ attention today, I don’t believe that this focus is their preference. In fact, read about physician burnout and exit of MDs from clinical practice to know today’s frenetic approach is not the reason most went into medicine.
I wonder if the vision for EMR facilitating integrated care was out of sync with the development of new delivery models and payment systems. It seems as if the currently available EMR approach was built as a billing tool in a fee-for-service model, not as a means of ensuring longitudinal care for patients.
Our scenario, like yours, was fortunate – available, knowledgeable, articulate children who advocated aggressively. Your question about “what about those who are less fortunate?” underscores the crisis – sadly, those people die, plain and simple.
Sue’s Thoughts: This breaks my heart!
You are correct in that your family has the education and sophistication to absorb and deal with these issues. Most families do not. They just fall between the cracks.
Sue’s Thoughts: Heart still breaking!
My mother-in-law was in a similar situation and were it not for my wife and her sister, it would have been a disaster. Nobody was in charge and with multiple physicians, decisions were made by one that were contrary to decisions made by another… Everyone has an interest in the status quo to protect their turf. I don’t believe the model can be repaired – it needs to be scrapped and rebuilt from [the] ground up. But how? It will be interesting to see how the JP Morgan, Amazon, Berkshire Hathaway entity builds itself out and whether it can manage to address the serious flaws in the current paradigm.
Sue’s Thoughts:
This was one of many connecting their very familiar personal experience. Let’s keep the conversation going, at both the big vision and the incremental change levels. Mostly, let’s make sure that we keep confirming the assumption that quality healthcare is a right and consistent with our values; just like education, roads, defense, and kindness.
If we don’t agree on that, the rest is not really worth talking about
P.S. Here is where we have come so far:
- Tales from the Healthcare Front Lines
- Planning for 2019 — Designing Effective Physician Advisory Board Meetings
- Rare Diseases: Abandon Everything You Think You Know
- Does Boston Biotech Have a Career Navigation Problem?
- Four Essential Market Assessment Questions
- Enjoy Summer, but Plan for the Fall
- The Sound of Silos
- When Did Process Become a Dirty Word?
- 21st Century Commercialization – More than a Point in Time!
- Power to the People
- Are You Getting the Most Out of Your Consultants?
- Nature vs. Nurture